CIRCULATORY DEATH AND DONATION (DCD)
WHAT IS DONATION AFTER
|
LEARN THE DIFFERENCE:
|
Imminent Death defined by CMS
• A patient:
• With severe, acute brain injury
• Who requires mechanical ventilation
• Who is in an ICU or Emergency Department
AND
• Has clinical findings consistent with a GCS that is less than or equal to a mutually-agreed-upon threshold (GCS <5)
OR
• Whose physicians are evaluating a diagnosis of brain death
OR
• Whose physician has ordered that life-sustaining therapies be withdrawn, pursuant to the family’s decision
DCD Defined
Organ procurement following pronouncement of death based on the irreversible cessation of circulatory functions.
• A patient:
• With severe, acute brain injury
• Who requires mechanical ventilation
• Who is in an ICU or Emergency Department
AND
• Has clinical findings consistent with a GCS that is less than or equal to a mutually-agreed-upon threshold (GCS <5)
OR
• Whose physicians are evaluating a diagnosis of brain death
OR
• Whose physician has ordered that life-sustaining therapies be withdrawn, pursuant to the family’s decision
DCD Defined
Organ procurement following pronouncement of death based on the irreversible cessation of circulatory functions.
HOW HOSPITAL STAFF PLAYS A ROLE IN DCD
Staff responsibilities vary depending on hospital DCD protocols, the individuals involved and the needs of the family. Here are some general guidelines:
PHYSICIAN
• Manages patient care
• Works to preserve life before judgment is made to withdraw support
• Serves as an advocate for the family and ensures families are offered the option of donation by LifeShare
• Once the family decides to proceed with donation, physician continues clinical management to preserve organ viability
in collaboration with LifeShare
• Physician will be present for withdrawal and declare patient’s death in the operating room or ICU
PHYSICIAN
• Manages patient care
• Works to preserve life before judgment is made to withdraw support
• Serves as an advocate for the family and ensures families are offered the option of donation by LifeShare
• Once the family decides to proceed with donation, physician continues clinical management to preserve organ viability
in collaboration with LifeShare
• Physician will be present for withdrawal and declare patient’s death in the operating room or ICU
|
NURSE
• Provides ongoing care to families throughout the patient’s hospitalization • Makes the referral call to LifeShare about the potential DCD donor • Coordinates the clinical management of the patient and support for the family in collaboration with LifeShare PASTORAL CARE AND SOCIAL SERVICES • Meets spiritual, religious and other needs of the patient and family • Serves as family advocate in collaboration with medical and nursing staff MAKE THE CALL 1-800-241-4483HOW THE DCD PROCESS WORKS |
The DCD process is no more difficult or complex than donation after brain death. The needs and wishes of the patient’s family are
always kept in focus by the medical team, by the LifeShare staff members and by social workers and clergy. The donation decision is made in the midst of enormous personal loss. Sensitivity, the willingness to listen and the ability to explain procedures in common terms can make organ donation an easier decision for families to make. It is a compassionate team effort.
always kept in focus by the medical team, by the LifeShare staff members and by social workers and clergy. The donation decision is made in the midst of enormous personal loss. Sensitivity, the willingness to listen and the ability to explain procedures in common terms can make organ donation an easier decision for families to make. It is a compassionate team effort.
|
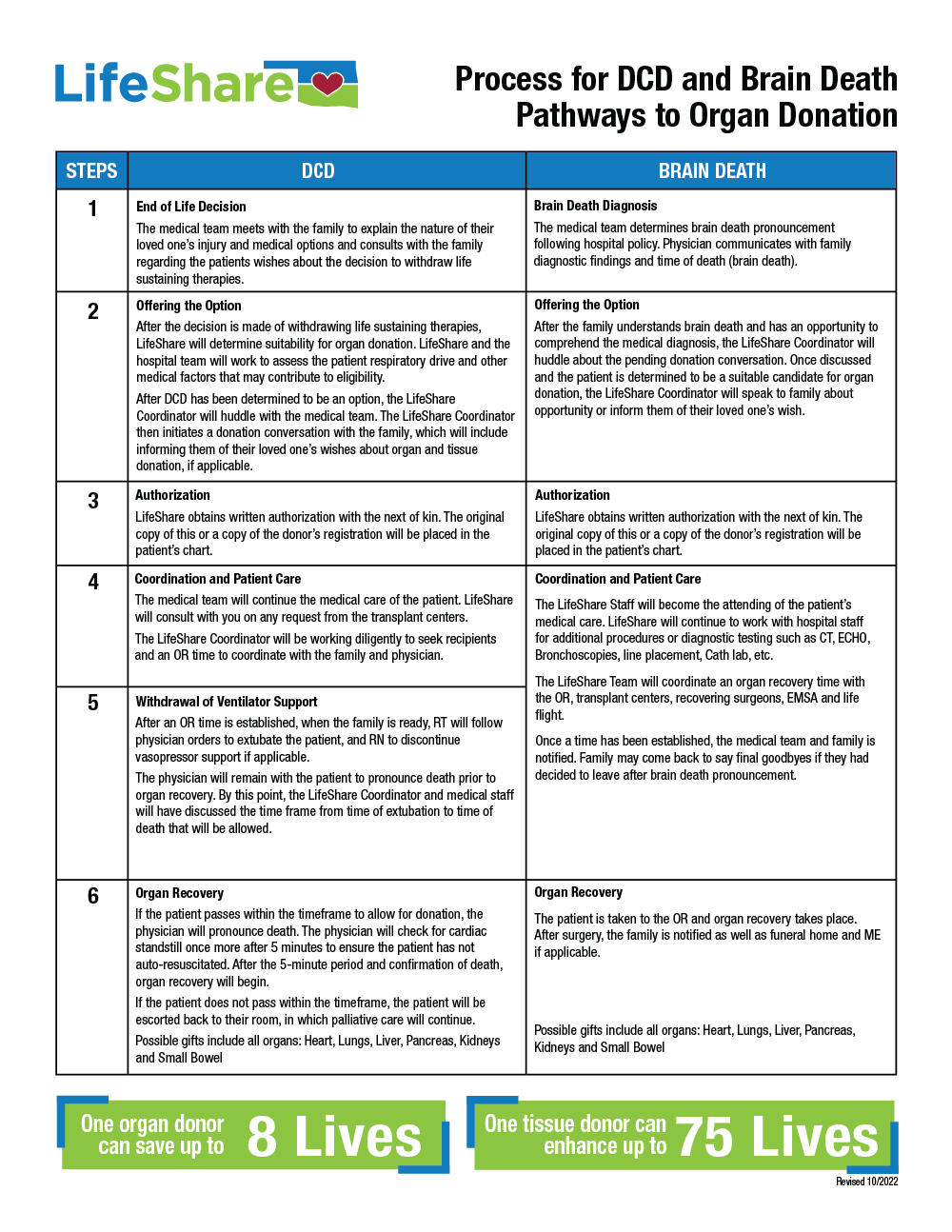
Step One
AN END-OF-LIFE DECISION For a patient with a severe brain injury, the medical team meets with the family to explain the nature of their loved one’s injury and prognosis. After exhausting all medical options, the medical team consults with the family regarding their wishes about the decision to withdraw life-sustaining therapies. The decision to withdraw support is made by the family and medical team. |
|
Step Two
OFFERING THE OPTION After the decision has been made to withdraw support, LifeShare determines the patient’s suitability for organ donation. LifeShare and the healthcare team will assess the patient’s respiratory drive and determine medical suitability. After LifeShare determines the patient may be a DCD candidate, a LifeShare representative approaches the family about donation or informs the family of their loved one’s wish. It is important to discuss donation in a quiet, private setting where the family feels most comfortable. The family should be assured that organ donation still allows for an autopsy, open-casket funeral or memorial service and that the donation will occur at no cost to them. Most importantly, the family should be told that their loved one’s donation will save lives. LifeShare coordinates the organ donation process. Timing of funeral arrangements is discussed. |
|
Step Three
AUTHORIZATION After the family has learned about their loved ones wishes or has agreed for them to be a donor, the next-of-kin completes the authorization form. LifeShare obtains written consent for several specific actions: • Organ Donation After Circulatory Death • Administration of medications to reduce clotting and improve organ function |
|
Step Four
EVALUATION LifeShare and the healthcare professionals at the hospital coordinate the donation process, including a respiratory drive assessment, organ function assessment and review of medical/social history. LifeShare schedules an operating room (OR) time and arranges for the surgical team to arrive. Additionally, LifeShare, staff and family discuss the possibility that the patient will not expire within the time frame needed for donation. Typically, this means the patient is returned to a unit for care and comfort measures. This does not mean the patient will get better, but that organ donation is not possible. Tissue donation may still be a possibility after death. |
|
Step Five
COORDINATION AND DECISION-MAKING LifeShare and medical staff, in consultation with the family, decide where support will be removed. This process typically occurs in an ICU. In some situations, it may take place in the operating room. This decision is made prior to arrival of the LifeShare surgical team. Withdrawal of support is usually done by the physician in charge of the patient's care. Depending on specific hospital policies and procedures, this also can be performed by an anesthesiologist, intensivist, on-call physician, resident or nurse. |
|
Step Seven
FINAL FAREWELL The family is given as much time as possible with their loved one. When the patient, hospital staff and family are ready, the hospital staff transfers the patient to the OR or prepares the ICU room for the withdrawal of support. When support is withdrawn in the ICU, the patient’s physician declares circulatory death and the team transfers the patient to the OR. If support is withdrawn in the OR, the following process takes place. |
|
Step Eight
WITHDRAWAL OF VENTILATOR SUPPORT During transfer, the patient is supported on a ventilator and monitored by the surgical team and hospital staff. The hospital staff member designated to withdraw support administers medications such as heparin and vasodilators. These medications prevent blood clotting and ensure good organ function. When the team is ready, the patient is extubated by the attending physician or his/her designee. The LifeShare surgical team cannot administer medications, withdraw support or declare death. As in all settings where support is withdrawn, comfort measures for the patient are of utmost importance. The attending physician may administer an analgesic based on his/her clinical judgment and in accordance with hospital policy, protocol or guidelines. The same end-of-life care is given to the patient regardless of whether support is withdrawn in the ICU or OR. |
|
Step Nine
ORGAN RECOVERY A hospital staff member declares death. The LifeShare surgical team waits an additional five minutes to ensure the patient’s heart does not start beating again. Research has shown that a patient’s heart will not start beating again beyond two minutes after the declaration of death. After waiting five minutes, organ recovery begins. If the patient does not expire within 60-90 minutes, the medical staff moves the patient to a location as outlined in Step Four and continues to administer palliative care. |