BRAIN DEATH AND DONATION
|
|
|
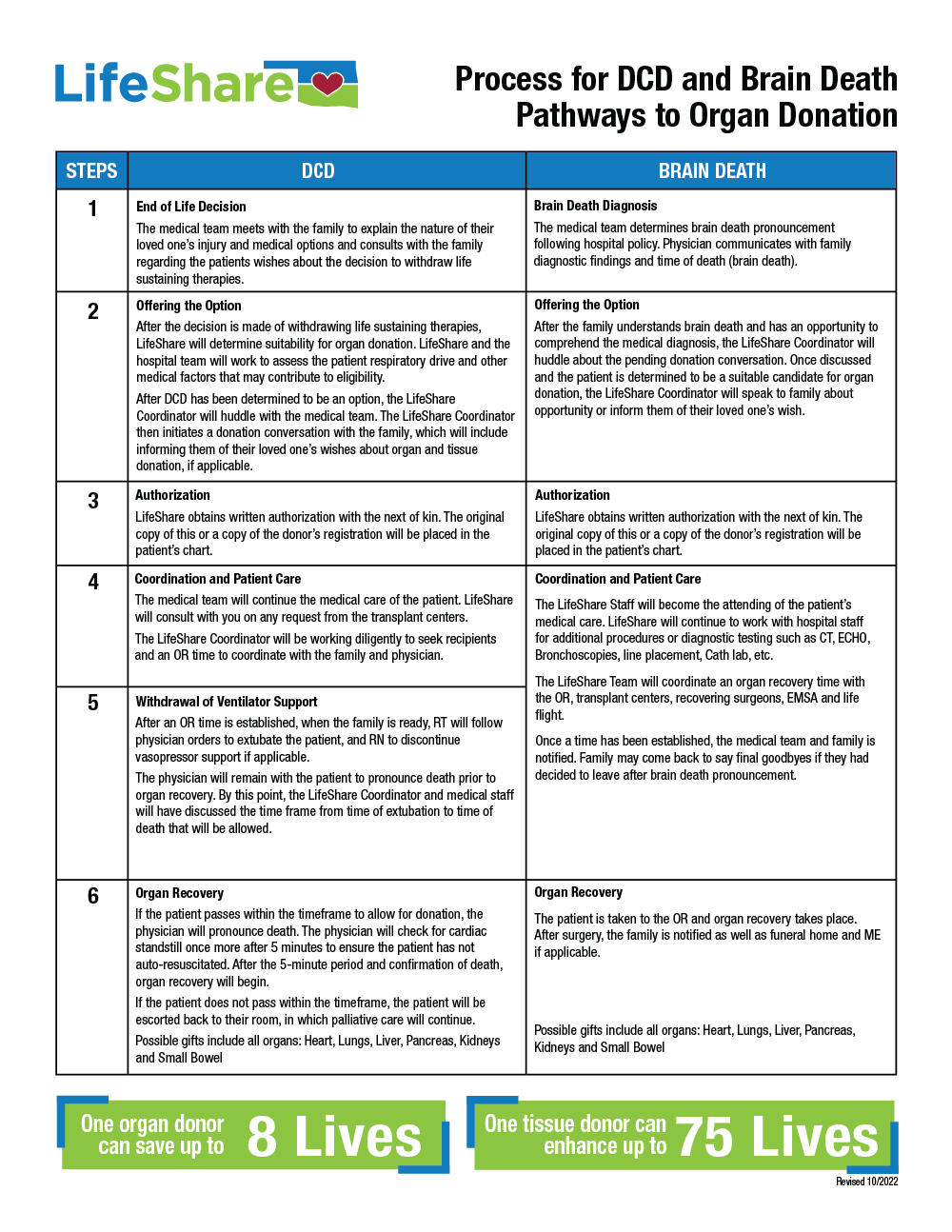
DONATION AFTER BRAIN DEATH (DBD) VS. DONATION AFTER CIRCULATORY DEATH (DCD)
Donation After Brain Death (DBD) |
Donation After Circulatory Death (DCD) |
|
TYPE |
Beating heart donor |
Deceased donor |
ANESTHESIA |
Anesthesia required |
Anesthesia may be required |
TIME FRAME |
Scheduled OR time - goes to OR on the vent |
Scheduled WDS time - OR staff available to help transport. Patient has a specified time frame to expire. After CTOD, rapid transport to OR for recovery. Hospital physician confirms death (5 minutes after CTOD) in the OR and recovery begins. *Process at some hospitals may be different* |
OR EQUIPMENT NEEDED |
Slush Machine x 2 Sternal Saw with Blade (test) Neptune or Dornoch Extra Back Tables x 2-5 Cautery Machine x 2 10” Long Vascular Clamp IV poles x 2-3 |
Slush Machine x 2 Sternal Saw with Blade (test) Neptune or Dornoch Extra Back Tables x 2-5 Cautery may be required 10” Long Vascular Clamp IV poles x 2-3 |
ORGANS RECOVERED |
Heart, lungs, liver, pancreas, kidneys and intestines |
Heart, lungs, liver, pancreas, kidneys and intestines |
HOW HOSPITAL STAFF PLAYS A ROLE IN BRAIN DEATH
Staff responsibilities vary depending on hospital protocols, the individuals involved and the needs of the family. Here are some general guidelines:
|
PHYSICIAN
• Manages patient care • Works to preserve life until brain death testing results have been completed • Physician declares patient’s brain death • Serves as an advocate for the family and ensures families are offered the option of donation by LifeShare • Physician continues clinical management to preserve organ viability in collaboration with LifeShare NURSE
• Provides ongoing care to families throughout the patient’s hospitalization • Makes the referral call to LifeShare about the potential donor • Coordinates the clinical management of the patient and support for the family in collaboration with LifeShare PASTORAL CARE AND SOCIAL SERVICES • Meets spiritual, religious and other needs of the patient and family • Serves as family advocate in collaboration with medical and nursing staff |
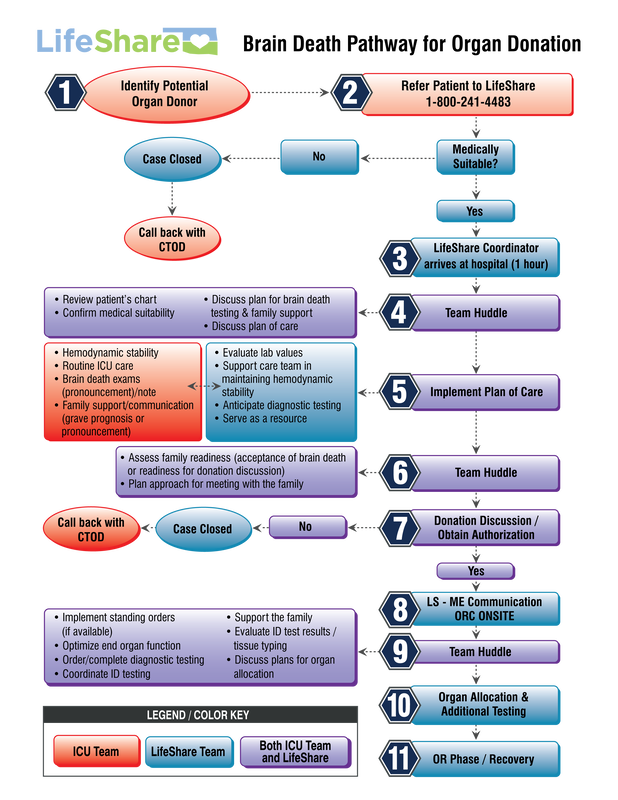
HOW THE BRAIN DEATH PROCESS WORKS
The needs and wishes of the patient’s family are always kept in focus by the medical team, by the LifeShare staff members and by social workers and clergy. The donation decision is made in the midst of enormous personal loss. Sensitivity, the willingness to listen and the ability to explain procedures in common terms can make organ donation an easier decision for families to make. It is a compassionate team effort.
|
Step Two
Testing for Brain Death When the medical team has exhausted all possible lifesaving efforts and the patient is not responding, a physician will perform a series of tests, usually on multiple occasions, to determine if brain death has occurred. Patients who are brain dead have no brain activity and cannot breathe on their own. Brain death is death and is irreversible. |
BRAIN DEATH DETERMINATION
The following are a summary of the American Academy of Neurology’s (AAN’s) Evidence-based Guidelines for Clinicians for determining Brain Death in Adults. The full guidelines are included in the back of this section.
PLEASE reference this hospital’s policy that addresses determination of brain death as it may differ from these guidelines.
Prior to exam, all of the following must be met according to AAN guidelines:
• Coma, irreversible and cause known
• Neuroimaging explains coma
• CNS depressant drug effect absent (if indicated toxicology screen; if barbiturates
given, serum level < 10µg/ml)
• No evidence of residual paralytics (electrical stimulation if paralytics used)
• Absence of severe acid-base, electrolyte, or endocrine abnormalities
• Normothermia (>36°C)
• Systolic blood pressure >100 mm Hg
• No spontaneous respirations
PLEASE reference this hospital’s policy that addresses determination of brain death as it may differ from these guidelines.
Prior to exam, all of the following must be met according to AAN guidelines:
• Coma, irreversible and cause known
• Neuroimaging explains coma
• CNS depressant drug effect absent (if indicated toxicology screen; if barbiturates
given, serum level < 10µg/ml)
• No evidence of residual paralytics (electrical stimulation if paralytics used)
• Absence of severe acid-base, electrolyte, or endocrine abnormalities
• Normothermia (>36°C)
• Systolic blood pressure >100 mm Hg
• No spontaneous respirations
BRAIN DEATH EXAMINATION
*All must be checked
• Pupils non-reactive to bright light
• Corneal reflex absent
• Oculocephalic reflex (dolls eyes) absent (tested only if C-spine integrity is ensured)
• Oculovestibular reflex absent (iced-caloric testing)
• No facial movements to noxious stimuli at supraorbital nerve, temporomandibular joint
• Gag reflex absent
• Cough reflex absent to tracheal suctioning
• Absence of motor response to noxious stimuli in all four limbs (spinally mediated reflexes are permissible)
When those have been evaluated and determined that reflexes are negative, then proceed with apnea test as part of the clinical exam.
• Apnea testing consistent with brain death
• If apnea is aborted or not performed because of hemodynamic instability, there must be a confirmatory test
ordered such as Nuclear Cerebral Blood Flow, EEG, Transcranial Doppler Scan, or Four Vessel Cerebral
Angiogram.
*Reference: AAN Guidelines
• Pupils non-reactive to bright light
• Corneal reflex absent
• Oculocephalic reflex (dolls eyes) absent (tested only if C-spine integrity is ensured)
• Oculovestibular reflex absent (iced-caloric testing)
• No facial movements to noxious stimuli at supraorbital nerve, temporomandibular joint
• Gag reflex absent
• Cough reflex absent to tracheal suctioning
• Absence of motor response to noxious stimuli in all four limbs (spinally mediated reflexes are permissible)
When those have been evaluated and determined that reflexes are negative, then proceed with apnea test as part of the clinical exam.
• Apnea testing consistent with brain death
• If apnea is aborted or not performed because of hemodynamic instability, there must be a confirmatory test
ordered such as Nuclear Cerebral Blood Flow, EEG, Transcranial Doppler Scan, or Four Vessel Cerebral
Angiogram.
*Reference: AAN Guidelines
BRAIN DEATH TESTING
Apnea Testing (CO2 Challenge)
• Prerequisites: 1) normotension, 2) normothermia, 3) euvolemia, 4) eucapnia (PaCO2 35-45 mm Hg), 5) absence of hypoxia, 6) no prior evidence of CO2 retention
• Adjust vasopressors to keep SBP >100 mm Hg
• Preoxygenate for at least 10 min with 100% FiO2
• Draw base line ABG to assess CO2 level
• Disconnect ventilator and place insufflation catheter through ET tube close to the carina. Deliver 100% O2 at 6L/min
• Observe for any spontaneous respirations for 8-10 min. If observed, abort test.
• If blood pressure or sats become unstable, abort test
• If no respiratory drive is observed, repeat ABG draw to assess CO2 level
• If CO2 increases by 20 mm Hg from an elevated baseline of >40mm Hg or is greater than or equal to 60 mm Hg if baseline pCO2 is normal, the apnea exam supports clinical diagnosis of brain death
Time of brain death should be determined when the arterial CO2 reached the target value. For patients that do not complete apnea testing, the time of death is when the ancillary test is clinically interpreted.
Pronouncing Brain Death
• One exam (clinical and apnea) is sufficient to pronounce brain death if done “several hours” from onset of insult in adult populations only. Two exams are expected for pediatric populations.
• Any physician can pronounce a patient brain dead in Oklahoma
o AAN suggests that physicians be familiar with and demonstrate competence in brain death pronouncement
• NOT mandatory but hospital policy may require confirmatory testing:
o Nuclear Brain Scan ( or Cerebral Blood Flow)
o Cerebral angiogram
o Transcranial Doppler Ultrasound
o EEG
• A physician’s death note should include date and time of death (DD/MM/YY) and the physician’s signature
o This is the time of death that gets reported to the Medical Examiner
Confirmatory Tests are Recommended when:
• Toxic levels of sedatives
• One or more brain stem reflexes cannot be tested:
o Severe facial trauma exists
o C-spine injury C4 or higher
o Pre-existing pupillary abnormalities
o Severe pulmonary disease resulting in CO2 retention
• Apnea test cannot be completed
*Reference: AAN Guidelines
• Prerequisites: 1) normotension, 2) normothermia, 3) euvolemia, 4) eucapnia (PaCO2 35-45 mm Hg), 5) absence of hypoxia, 6) no prior evidence of CO2 retention
• Adjust vasopressors to keep SBP >100 mm Hg
• Preoxygenate for at least 10 min with 100% FiO2
• Draw base line ABG to assess CO2 level
• Disconnect ventilator and place insufflation catheter through ET tube close to the carina. Deliver 100% O2 at 6L/min
• Observe for any spontaneous respirations for 8-10 min. If observed, abort test.
• If blood pressure or sats become unstable, abort test
• If no respiratory drive is observed, repeat ABG draw to assess CO2 level
• If CO2 increases by 20 mm Hg from an elevated baseline of >40mm Hg or is greater than or equal to 60 mm Hg if baseline pCO2 is normal, the apnea exam supports clinical diagnosis of brain death
Time of brain death should be determined when the arterial CO2 reached the target value. For patients that do not complete apnea testing, the time of death is when the ancillary test is clinically interpreted.
Pronouncing Brain Death
• One exam (clinical and apnea) is sufficient to pronounce brain death if done “several hours” from onset of insult in adult populations only. Two exams are expected for pediatric populations.
• Any physician can pronounce a patient brain dead in Oklahoma
o AAN suggests that physicians be familiar with and demonstrate competence in brain death pronouncement
• NOT mandatory but hospital policy may require confirmatory testing:
o Nuclear Brain Scan ( or Cerebral Blood Flow)
o Cerebral angiogram
o Transcranial Doppler Ultrasound
o EEG
• A physician’s death note should include date and time of death (DD/MM/YY) and the physician’s signature
o This is the time of death that gets reported to the Medical Examiner
Confirmatory Tests are Recommended when:
• Toxic levels of sedatives
• One or more brain stem reflexes cannot be tested:
o Severe facial trauma exists
o C-spine injury C4 or higher
o Pre-existing pupillary abnormalities
o Severe pulmonary disease resulting in CO2 retention
• Apnea test cannot be completed
*Reference: AAN Guidelines