CLINICAL TRIGGERS FOR TIMELY REFERRALS
|
|
Understanding Clinical Triggers for Organ Donation presented by Taylor Risenhoover, R.N. |
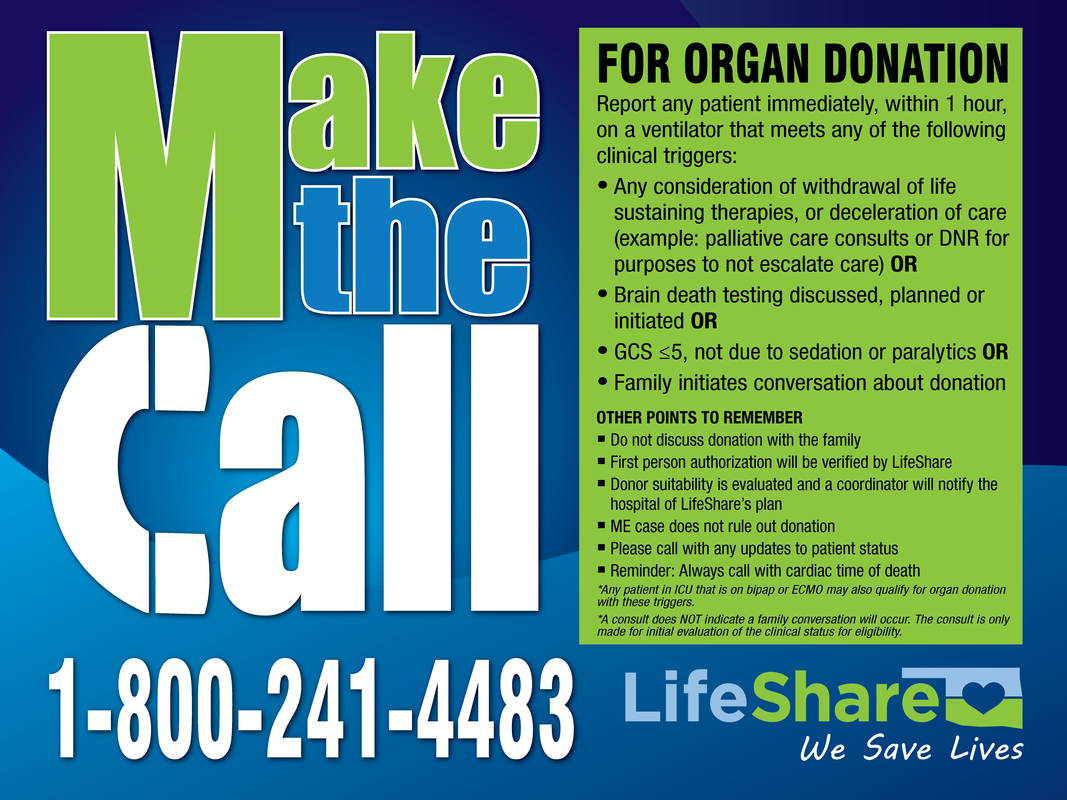
TIMELY REFERRAL CRITERIA* FOR ORGAN DONATION
Report any patient immediately (within 1 hour) on a ventilator that meets any of the following clinical triggers:
• Any consideration of withdrawal of life sustaining therapies, or deceleration of care (example: palliative care consults OR DNR for purposes to not escalate care) OR
• Brain death testing discussed, planned or initiated OR
• GCS < 5, not due to sedation or paralytics OR
• Family initiates conversation about donation
• Brain death testing discussed, planned or initiated OR
• GCS < 5, not due to sedation or paralytics OR
• Family initiates conversation about donation
*Any patient in ICU that is on bipap or ECMO may also qualify for organ donation with these triggers.
*A consult does NOT indicate a family conversation will occur. The consult is only made for initial evaluation of the clinical status for eligibility.
*A consult does NOT indicate a family conversation will occur. The consult is only made for initial evaluation of the clinical status for eligibility.
WHEN TO UPDATE THE DONOR REFERRAL
• Changes in patient code status
• Declines in patient's neurological status
• When there are plans to discuss withdrawal of support to allow natural death
• A cardiac time of death, even when previously referred for organ donation
• Declines in patient's neurological status
• When there are plans to discuss withdrawal of support to allow natural death
• A cardiac time of death, even when previously referred for organ donation
REMEMBER: WAIT, DON'T EXTUBATE MAKE THE CALL 1-800-241-4483
• Do not discuss donation with the family
• First person authorization will be verified by LifeShare
• Donor suitability is evaluated and a coordinator will notify the hospital of LifeShare’s plan
• ME case does not rule out donation
• Please call with any updates to patient status
• Reminder: Always call within 60 minutes of cardiac time of death
• First person authorization will be verified by LifeShare
• Donor suitability is evaluated and a coordinator will notify the hospital of LifeShare’s plan
• ME case does not rule out donation
• Please call with any updates to patient status
• Reminder: Always call within 60 minutes of cardiac time of death
*This criteria meets Center for Medicare & Medicaid Services regulations pertaining to organ and tissue donation.
GLASGOW COMA SCALE
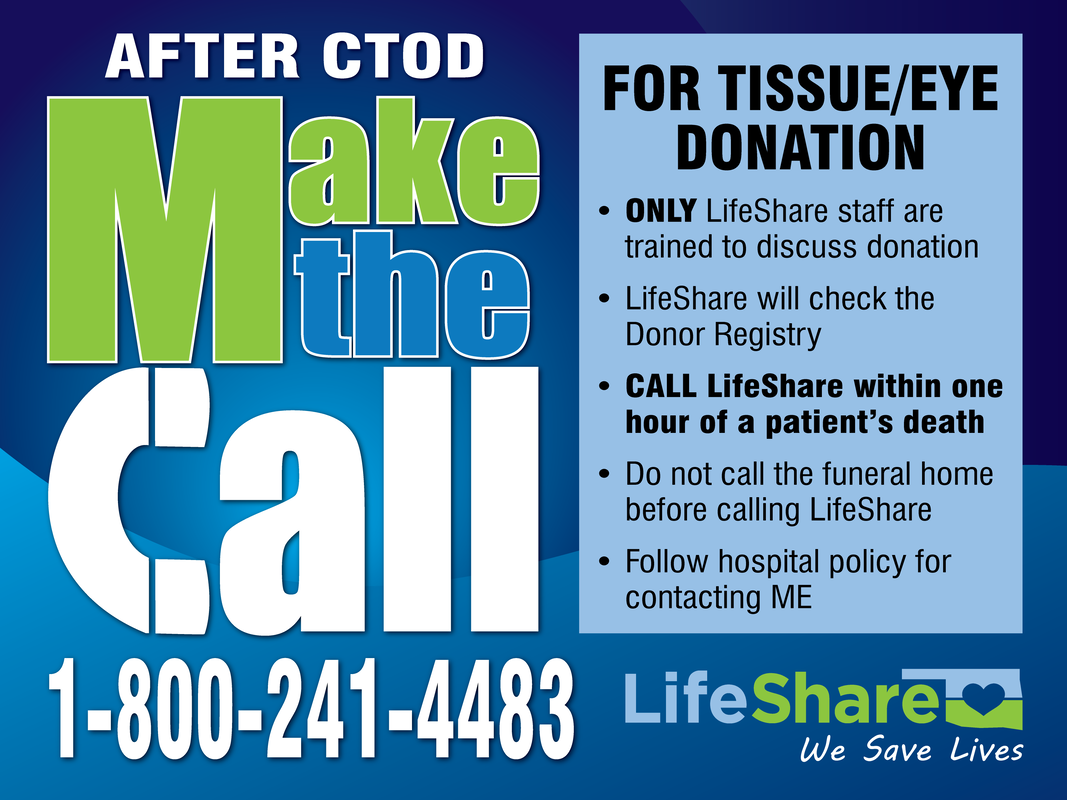
TIMELY TISSUE REFERRAL CRITERIA* FOR TISSUE DONATION
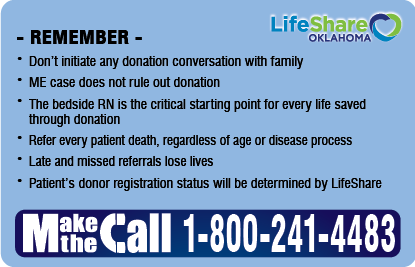
MAKE THE CALL 1-800-241-4483
• Call on EVERY death
• Call within ONE HOUR of patient's death
• DO NOT call the funeral home until after speaking with the LifeShare Coordinator
• DO NOT initiate any donation conversation with family
• ME case DOES NOT rule out donation
• The bedside RN is the critical starting point for every life saved through donation
• Refer every patient death, regardless of age or disease process
• Late and missed referrals lose lives
• Patient's donor registration status will be determined by LifeShare
• Call within ONE HOUR of patient's death
• DO NOT call the funeral home until after speaking with the LifeShare Coordinator
• DO NOT initiate any donation conversation with family
• ME case DOES NOT rule out donation
• The bedside RN is the critical starting point for every life saved through donation
• Refer every patient death, regardless of age or disease process
• Late and missed referrals lose lives
• Patient's donor registration status will be determined by LifeShare
*This criteria meets Center for Medicare & Medicaid Services regulations pertaining to organ and tissue donation.
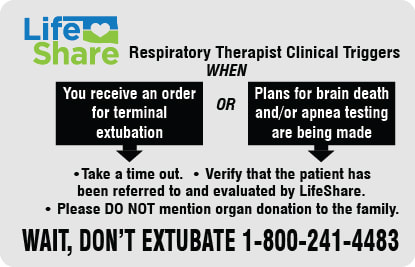
RESPIRATORY THERAPIST CLINICAL TRIGGERS
• When you receive an order for terminal extubation
OR
• Plans for brain death and/or apnea testing are being made
• Take a time out
• Verify that the patient has been referred to and evaluated by LifeShare
• DO NOT initiate any donation conversation with family
OR
• Plans for brain death and/or apnea testing are being made
• Take a time out
• Verify that the patient has been referred to and evaluated by LifeShare
• DO NOT initiate any donation conversation with family
REMEMBER: WAIT, DON'T EXTUBATE MAKE THE CALL 1-800-241-4483
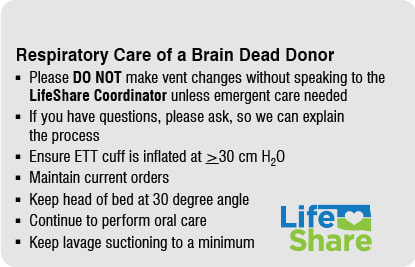
RESPIRATORY CARE OF A BRAIN DEAD DONOR
• Please DO NOT make vent changes without speaking to the LifeShare Coordinator unless emergent care needed
• If you have questions, please ask, so we can explain the process
• Ensure ETT cuff is inflated at >30 cm H2O
• Maintain current orders
• Keep head of bed at 30 degree angle
• Continue to perform oral care
• Keep lavage suctioning to a minimum
• If you have questions, please ask, so we can explain the process
• Ensure ETT cuff is inflated at >30 cm H2O
• Maintain current orders
• Keep head of bed at 30 degree angle
• Continue to perform oral care
• Keep lavage suctioning to a minimum
DONATION AFTER BRAIN DEATH (DBD) VS. DONATION AFTER CIRCULATORY DEATH (DCD)
c |
Donation After Brain Death (DBD) |
Donation After Circulatory Death (DCD) |
TYPE |
Beating heart donor |
Deceased donor |
ANESTHESIA |
Anesthesia required |
Anesthesia may be required |
TIME FRAME |
Scheduled OR time - goes to OR on the vent |
Scheduled WDS time - OR staff available to help transport. Patient has a specified time frame to expire. After CTOD, rapid transport to OR for recovery. Hospital physician confirms death (5 minutes after CTOD) in the OR and recovery begins. *Process at some hospitals may be different* |
OR EQUIPMENT NEEDED |
Slush Machine x 2 Sternal Saw with Blade (test) Neptune or Dornoch Extra Back Tables x 2-5 Cautery Machine x 2 10” Long Vascular Clamp IV poles x 2-3 |
Slush Machine x 2 Sternal Saw with Blade (test) Neptune or Dornoch Extra Back Tables x 2-5 Cautery may be required 10” Long Vascular Clamp IV poles x 2-3 |
ORGANS RECOVERED |
Heart, lungs, liver, pancreas, kidneys and intestines |
Heart, lungs, liver, pancreas, kidneys and intestines |
OPERATING ROOM
• Surgical Recovery Coordinator (SRC) will arrive 1.5 hours before case to help set up and answer questions
• OR needs to be open and ready to go for all DCDs prior to WDS/extubation
• Circulator and anesthesia will assist in transporting donor to OR
• Prep and drape
• Time out performed by circulator
• LifeShare staff will perform a Moment of Silence for the donor
After Cross Clamp
• SRC will start flushing organs to start preservation process
• Anesthesia will turn off the anesthesia machine
• Order of operation: Heart, Lungs, Liver, Pancreas, Kidneys, Intestines unless organ is going for research. Research organs are recovered last.
• SRCs are responsible for identifying anatomy, dissecting, cannulating renal arteries, and placing kidneys on pump
• If a medical examiner case, all lines will be left in place
• OR needs to be open and ready to go for all DCDs prior to WDS/extubation
• Circulator and anesthesia will assist in transporting donor to OR
• Prep and drape
• Time out performed by circulator
• LifeShare staff will perform a Moment of Silence for the donor
After Cross Clamp
• SRC will start flushing organs to start preservation process
• Anesthesia will turn off the anesthesia machine
• Order of operation: Heart, Lungs, Liver, Pancreas, Kidneys, Intestines unless organ is going for research. Research organs are recovered last.
• SRCs are responsible for identifying anatomy, dissecting, cannulating renal arteries, and placing kidneys on pump
• If a medical examiner case, all lines will be left in place
*This criteria meets Center for Medicare & Medicaid Services regulations pertaining to organ and tissue donation.